Chipping Away at Avoidable Days: How Even Small Improvements in Patient Length of Stay Add Up
For hospitals and health systems seeking to maximize revenue and resource utilization while providing an impeccable patient experience, any unnecessary extension of the patient’s stay can dramatically hinder performance.
Imagine that each step in the patient’s journey at your institution is a link in a chain.
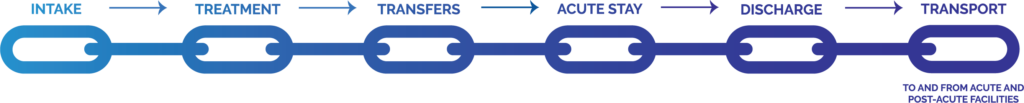
If each of these steps is a link in the chain, then any additional time a patient spends at one of those links is indicative of a break in that chain. Let’s take, for instance, the transfer between departments within a health system. No matter if that transfer is delayed due to reliance on manual processes, overtaxed staff members or a lack of available bed space in the ward the patient is moving to, the result is the same: patients potentially spending more time than necessary at stops along their care journey.
Let’s imagine a cardiac patient, David, who has been stabilized and ready for a transition from the the ICU to telemetry. If David cannot be moved because telemetry beds are all full, it causes a ripple effect up and down the patient population. And while David remains unnecessarily in the ICU, that’s a bed that could have been provided to another incoming patient presenting cardiac symptoms – let’s call her Cynthia – and she too experiences a delay.
Avoidable days are the culmination of these delays. Taken at scale, and across the full continuum of patient care, these kinds of delays add up to a staggering amount of lost revenue across a health system – and can have serious consequences for patient care.
It doesn’t even take full days for these numbers to add up. Even fractions of a day lost are enough to cause revenue headaches for your organization.
So how do you wrest this time, and revenue, back from the brink? How do you ensure that a single broken link in the chain doesn’t result in substantial loss for your health system?
Patient Access Centers Bring Visibility, Navigability and Accountability to the Patient Journey
To bring order to the patient journey, and thus reduce the threat of avoidable days, you need to understand where there might be shortfalls within your organization. And that’s where an access center comes into play.
The access center acts as a repository of all the information related to patient care and patient movement, as well as data related to resource utilization across their journey. By unifying streams of data from across departments and accounting for the totality of the patient experience, health systems that establish a patient access center can begin the process of identifying broken links in the chain and take steps to correct those issues.
Let’s imagine that you’re able to quickly identify that the issue lies not with capacity, but with the transfer process between departments. By analyzing the data at a high level and then zooming in on areas of deficiency, it turns out that a speedy transfer between departments is encumbered by a reliance on nurses being asked to make calls to different points within the hospital in order to coordinate pick-up and arrival of the patient to their new space.
In this scenario, multiple problems can be pointed out: a nurse may not be the ideal person to place these calls, because he or she is conducting an administrative task rather than overseeing the provision of care they’re licensed for, preventing top-of-license utilization of that staff member. The calls themselves rely on someone in the other department to answer or return a voicemail, thus a successful transfer is contingent on someone else’s time. And calling may not be the most efficient means of transfer, as automated software solutions at the point of care could facilitate this process more quickly.
The patient access center identifies the break in the chain, and analysis by a clinical expert well-versed in these concepts can take a closer look to correct the issue. Three possible reasons for the problem were identified, and you can thus begin deploying solutions.
Hiring a separate individual to focus exclusively on patient transfers? Good, but not great, as you then need to deal with everything that comes along with hiring a new person, eating into your potential revenue recovery. Removing the phone call from the situation entirely? Now you’re in business. If you can remove a manual portion of the process and replace it with an automated solution that can accomplish the same thing with a few clicks, you’ve made real progress.
This is but one example; coordinating data across the spectrum of patient care and centralizing it within the patient access center can and will identify numerous areas just like this. Each solution reduces avoidable days and enables you to reclaim lost revenue. Over time, you’ll be able to refine these processes even further, and you’ll wonder how so many avoidable days ever accumulated in the first place.
We’ve covered a lot of ground, but hopefully you’ve gotten a sense of just how widespread the problem of avoidable days is and how even seemingly minor delays can have a cumulative effect. By minimizing these delays with a patient access center and everything it allows you to accomplish, you can reclaim revenue and identify opportunities for further gain that you never could have anticipated.